You’re having a fun mukbang session with your friends, laughing and eating your heart out, when suddenly, that fiery burn creeps up your chest. Or maybe you’re enjoying your afternoon coffee ritual, savoring every sip, only for that comforting warmth to turn into a slow, uncomfortable sensation in your throat. You pause and wonder, what’s happening?
One friend might casually tell you, “That’s just heartburn.” Your parents may call it acid reflux, while you start Googling GERD symptoms, convinced that’s the culprit.
The truth is, heartburn, acid reflux, and GERD are connected but not identical. Heartburn is a symptom, acid reflux is a process, and GERD is a chronic condition that shouldn’t be ignored. Understanding the difference matters, not only so you can describe your symptoms accurately but also so you can take steps to manage or prevent them.
Before you pop over-the-counter antacids or scroll the web in panic, here’s a simple breakdown of these three commonly mixed-up terms
The Burning Question: Aren’t They the Same?
Stop mixing them up. Here’s a simple way to tell these three conditions apart:
Heartburn: The Symptom You Feel
Heartburn isn’t a condition on its own! It is a symptom. It often feels like a fiery pain that starts in your chest and creeps up toward your throat. Moreover, it often strikes after large meals or foods high in spice, fat, or acidity, like tomatoes, citrus fruits, and fried dishes.
Over time, frequent heartburn can lead to dysphagia, or difficulty swallowing. This occurs when repeated acid exposure irritates and inflames the esophagus, sometimes causing swelling or scarring that narrows the passageway. As a result, swallowing may feel uncomfortable, as if food is getting stuck or moving down more slowly than usual.
Occasional heartburn isn’t usually a big deal, but frequent flare-ups may mean you’re dealing with acid reflux or a more chronic issue like GERD (Gastroesophageal Reflux Disease).
Acid Reflux : The Actual Process
You already know that heartburn happens when acid goes up into your esophagus, but what’s really going on inside your stomach? Acid reflux is the process causing that discomfort. It happens when your lower esophageal sphincter (LES, the muscle that acts like a gate between your esophagus and stomach) relaxes or weakens at the wrong time. Normally, it stays tightly closed to keep your food and stomach acid where they belong, but when it doesn’t close properly, acid escapes upward, irritating your throat and esophagus.
That burning feeling isn’t the only sign of reflux. You might notice a sour or bitter taste in your mouth after eating, or find yourself clearing your throat constantly. Some people can have acid reflux without ever feeling heartburn, which can make it challenging to spot.
GERD: The Chronic Illness
Gastroesophageal reflux disease (GERD) is what happens when acid reflux becomes frequent. If you have reflux symptoms more than twice a week, or if your discomfort is interfering with daily life, you may have GERD. Over time, untreated GERD can lead to complications like:
● Esophagitis: Inflammation of the esophagus
● Strictures: Narrowing of the esophagus due to scarring
● Barrett’s Esophagus: Precancerous changes in the esophageal lining
GERD isn’t something to ignore. While acid reflux is common, chronic exposure to stomach acid can damage your esophagus and even increase your risk of serious conditions.
Heartburn, Reflux, GERD: Explained in 3 Lines
Before getting into some tips, here’s a cheat sheet on the relationship between the three conditions:
● Heartburn is the burning symptom you feel.
● Acid reflux is the process that causes heartburn (acid moving up into your esophagus).
● GERD is when acid reflux becomes a chronic disease that needs medical attention.
Ways to Help Ease the Discomfort
While these three terms, heartburn, acid reflux, and GERD, aren’t the same, they can all disrupt your daily routine and affect your quality of life. The silver lining? You don’t have to let occasional discomfort turn into a bigger issue. With a few simple lifestyle changes, you can help ease that burning sensation and take control of your digestive health.
Here are some quick tips to help you feel better:
1. Watch What You Eat and Drink
Spicy food, coffee, alcohol, and fatty meals are some of the most common triggers of heartburn. Try keeping a food journal to spot your personal culprits, and cut back on foods that cause flare-ups.
2. Eat Smaller, Slower Meals
Overeating puts pressure on your stomach, making it easier for acid to escape into your esophagus. Eat smaller portions and chew your food thoroughly.
3. Stay Upright After Meals
Lying down right after eating can worsen heartburn. Instead, stay upright for at least 2-3 hours after meals to let gravity help keep stomach acid where it belongs.
4. Elevate Your Head While Sleeping
If nighttime heartburn is keeping you up all night, consider sleeping with extra pillows under your upper body. This position makes it harder for acid to creep up while you sleep.
5. Maintain a Healthy Weight and Lifestyle
Excess weight around your midsection increases pressure on your stomach. Pairing mindful eating with regular exercise can help reduce heartburn episodes over time.
When Lifestyle Changes Aren’t Enough
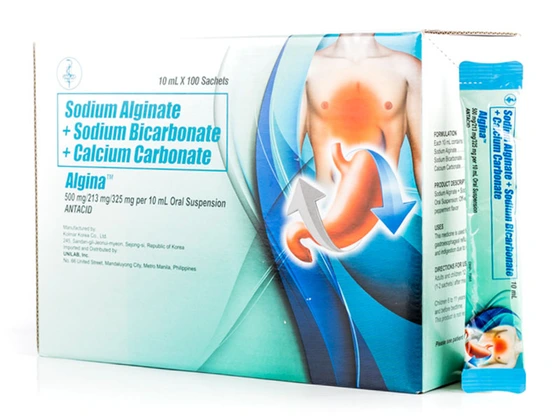
Even with these tips, there may be times when the pain strikes and you need relief. That’s where over-the-counter antacids like Sodium Alginate + Sodium Bicarbonate + Calcium Carbonate (Algina™) can help.
Sodium Alginate + Sodium Bicarbonate + Calcium Carbonate (Algina™) is used to help treat symptoms of gastroesophageal reflux such as acid regurgitation, heartburn, and indigestion due to reflux of stomach contents.
How much and how often should you use this medicine?
For adults and children aged 12 years and older: Take 10–20 mL (1–2 sachets) after meals and at bedtime. You can take Sodium Alginate + Sodium Bicarbonate + Calcium Carbonate (Algina™) up to four times daily.
Children 6 to 11 years old: Take 5 to 10 mL (1 sachet) after meals and before bedtime.
Sodium Alginate + Sodium Bicarbonate + Calcium Carbonate (Algina™) is not recommended for children under 6 years old.
If symptoms persist, consult a doctor.
References:
https://my.clevelandclinic.org/health/diseases/9617-heartburn-overview
https://www.nhs.uk/conditions/heartburn-and-acid-reflux/
https://pmc.ncbi.nlm.nih.gov/articles/PMC3975977/
https://pmc.ncbi.nlm.nih.gov/articles/PMC6970278/
https://www.massgeneralbrigham.org/en/about/newsroom/articles/heartburn-vs-heart-attack-how-to-tell-the-difference
https://www.missionhealth.org/healthy-living/blog/is-it-heartburn-or-heart-attack#:~:text=There%20are%20a%20few%20ways,the%20back%2C%20jaw%20and%20neck.
https://my.clevelandclinic.org/health/diseases/17019-acid-reflux-gerd
ASC Ref No. U0274P090925A